HPV is Not in Scarlet Letters: Cervical Cancer Patients Being Stigmatized

By Kathleen Hoffman, PhD, MSPH
Imagine being given a diagnosis of cervical cancer. That’s bad enough. Now, imagine that it comes with the assumption you got it by sleeping around.
In 1983 and 1984, Dr. Harold zur Hausen isolated Human Papillomavirus (HPV). There are more than 200 types of human papillomavirus (HPV), most of which are common and symptom-free.1 But several variants, HPV-16 and HPV-18 being the first two identified, are associated with cervical cancer. HPV-16 is in 50 percent of cancers and HPV-18 in 20 percent of cervical cancers, respectively.2 Years of research resulted in approval of an HVP vaccine for females in 2006; it took almost four more years for the same vaccine to be approved for males.3
Before then, the only association the public made with HPV, if at all, was that it causes genital warts. But now people who have been diagnosed with cancer are burdened with the assumption of having a sexually transmitted disease.
Each year, more than 13,000 women are diagnosed with cervical cancer in the United States according to the National Cervical Cancer Coalition (a program of the American Sexual Health Association).4
The National Cervical Cancer Coalition website explains,
“After being diagnosed, some people feel like they are the only person they know with HPV. It’s easy to understand why so many people hold this misunderstanding. After all, public awareness of the virus is extremely low.” 4
Although awareness is low, the Human Papilloma Virus (HPV) is extremely common. Of all people in the US age 15 to 49, between 75 and 80 percent have had HPV.1 It’s the most common sexually transmitted infection. Yet in a study published in 2018, involving in-depth interviews with patients being treated for HPV-related cancers, patients did not understand HPV’s role in their cancer and most didn’t even mention HPV as causally related to their cancer. 5
But there is evidence of non-sexual HPV transmission. Indeed, vertical transmission from mother to baby is possible.6 Additionally, HPV has been found to be highly resistant to disinfectants. HPV DNA has been found on reusable ultrasound probes used in transvaginal, transrectal, and trans-esophogeal ultrasound medical procedures.7
The National Cervical Cancer Coalition Support Community on Inspire
Members of the National Cervical Cancer Coalition Support Community on Inspire write about their experiences with feeling isolated with their HPV-positive diagnosis or with having cervical cancer.
“I often times feel so alone its crippling…. I haven’t told my family because I don’t want them to see me differently or get upset.”
Another member wrote,
“you are made to feel dirty from having caught HPV. I went to a gyn for a second opinion and the man actually said that having a lot of sex partners was how most people got this virus. I wanted to slap him. I explained that no some women or girls can be virgins or marry their first love and get this virus…, I was angry that this man was judging me or other women like it was all our fault. That the man was not responsible for anything.”
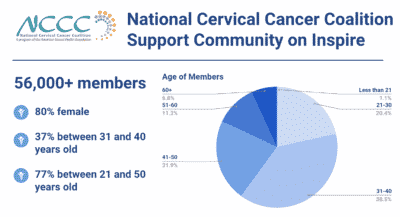
There are over 56,000 members in the National Cervical Cancer Coalition Support Community on Inspire. Eighty percent are female. Thirty-seven percent are between 31 and 40 years old. Overall 77 percent are between 21-50 years old. 8
A study published in 2013 looked at stigma felt by women infected with HPV and men infected by HPV. The study found greater association of negative emotions and stigma among women than among men. 9 The results of a search on the word “stigma” in this community yielded 399 posts. Three hundred thirty-four posts resulted in the search for “HPV embarrassment.” 8
As one member stated,
“With all this HPV stuff. WHY….are only women dealing with this. WHY is it our burden. WHY, do the Doctors look at you and say “Have you been with alot of men?” Like b/c I have HPV I am sleeping around…it all seems unfair and I am starting to feel like HPV, Dsyplasia and Cervical Cancer is starting to get viewed as bad in society now. Like we should be embarrassed.”
Another posted,
“I was recently diagnosed with adenocarcinoma …the HPV stigma [is] a little out of control. It is humiliating …calling this a “preventable” cancer is difficult to deal with…. Everyone should be told that this is not a disease of deviants….it can happen to anyone and it does.”
The repercussions of disease related stigma cannot be underestimated. It is associated with decreased interest in getting screenings, reduced access to social support and reluctance to get treatment.
Hopelessness and self-loathing
A 2010 study used quantitative survey and in-depth interviews to learn how an abnormal Pap smear and HPV positive diagnosis impacted patients. Researchers found patients experienced self-blame, fear, stigma, feelings of powerlessness and anger. 10
Women in the National Cervical Cancer Coalition Support Community on Inspire express these same emotions. They describe feeling hopeless and experiencing self-loathing.
“Is it normal to have HPV for more than _#_ years. …I feel alone so alone in this… I am dealing with a “no solution” disease. I feel like I have AIDs I feel like I will have cancer. I wish I knew what I could …to avoid the inedible.[inevitable] I haven’t spoken to my family or friends about this because it will put so much stress on them and pressure on me to disclose this information…On top of it all I feel embarrassed and disgusted in myself.”
Another wrote,
“When I first learned I had HPV, although I didn’t automatically know what it was, I felt dirty.”
Yet another stated,
“I am really struggling with ways not to feel like damaged goods for the rest of my life.”
Women in long-term relationships
In a qualitative study in England, researchers conducted one-on-one interviews and a focus group with women who had just received positive HPV results with abnormal pap smears and women who had not. Women in long-term relationships who did not have a diagnosis were certain that “nothing would be found” while those who were HPV positive had trouble coming to terms with the diagnosis, articulating shock, embarrassment and trying to figure out how they could have been infected. Those who had had only one sexual partner felt they were not at risk and didn’t understand that their partners status could impact their health. 11
Members of the Inspire community also experienced shock.
“Here I am, happily married for _#_ years, _#_ kids, _#_ years old, and now I find out I have a sexually transmitted disease? Are you kidding me? I am so traumatized…I think the HVP bothers me worse than my [abnormal pap smear]. I mean in the sense that if this were any other kind of illness, I could talk to my mom, my friends, maybe my co-workers. I have not spoken about this to anyone, except my husband”
Another member responded,
“My husband and best friend know about the phone call/test and that it’s most likely HPV. Your post resonated with me since I’m _#_ , married for _#_ years, and have _#_ kids…. What I can’t seem to find anywhere on the Internet is the answer to “now what?” Aside from the various medical procedures I will likely undergo, I don’t know what day-today life will bring…not knowing what my “new normal” is going to be is driving me crazy”
What’s Next?
Perhaps the stigma that women have experienced will begin to diminish as the truth about this pervasive virus is shared and more people are vaccinated. In October 2018, the FDA expanded the age of HPV vaccinations to 45 years for both women and men.12
In the meantime, the National Cervical Cancer Coalition website provides an eBook, HPV & Cervical Cancer: Stories from Survivors and Supporters. The website provides access to a toll free number, videos, in-person support groups and information and of course, an online support community on Inspire.4
Inspire offers a trusted community to patients and caregivers. Our goal with this blog, this website and our content is to provide the life science industry access to the true, authentic patient voice. In so doing, we support faithful operationalization of patient-centricity. Take a look at our case studies, eBooks and news outlet coverage.
References
1 https://www.plannedparenthood.org/learn/stds-hiv-safer-sex/hpv
2 https://www.nobelprize.org/prizes/medicine/2008/hausen/biographical/
3 Chaturvedi, A. Graubard, B. Broutian, T., (2018) Effect of Prophylactic Human Papillomavirus (HPV) Vaccination on Oral HPV Infections Among Young Adults in the United States J Clin Oncol. 36(3): 262–267.doi: 10.1200/JCO.2017.75.0141
4 https://www.nccc-online.org
5 Best, A. Logan,R. Vázquez-Otero,C. et al. (2018) Application of a Health Literacy Framework to Explore Patients’ Knowledge of the Link between HPV and Cancer, Journal of Health Communication,23:8, 695-702, DOI: 10.1080/10810730.2018.1508257
6 Lee, S. Park,J. Norwitz, E. et al. (2013) Risk of Vertical Transmission of Human Papillomavirus throughout Pregnancy: A Prospective Study. PLoS One. 8(6): e66368.doi: 10.1371/journal.pone.0066368
7 Ryndock, E. & Meyers, C. (2014) A risk for non-sexual transmission of human papillomavirus?, Expert Review of Anti-infective Therapy, 12:10, 1165-1170, DOI: 10.1586/14787210.2014.959497
8 https://www.inspire.com/groups/national-cervical-cancer-coalition/
9 Daley, E. Vamos, C. Wheldon, C. (2015). Negative emotions and stigma associated with a human papillomavirus test result: A comparison between human papillomavirus–positive men and women, Journal of Health Psychology, 20(8), 1073–1082. https://journals.sagepub.com/doi/abs/10.1177/1359105313507963
10 Daley, E. Perrin, K. McDermott, J. (2010). The psychosocial burden of HPV: a mixed-method study of knowledge, attitudes and behaviors among HPV+ women. Journal of Health Psychology, 15(2):279-90. Doi: 10.1177/1359105309351249.
11 Patel, H. Moss, E., Sherman, S. (2018). HPV primary cervical screening in England: Women’s awareness and attitiudes. Psycho-Oncology 27(6): 1559-1565.
12 https://www.fda.gov/news-events/press-announcements/fda-approves-expanded-use-gardasil-9-include-individuals-27-through-45-years-old