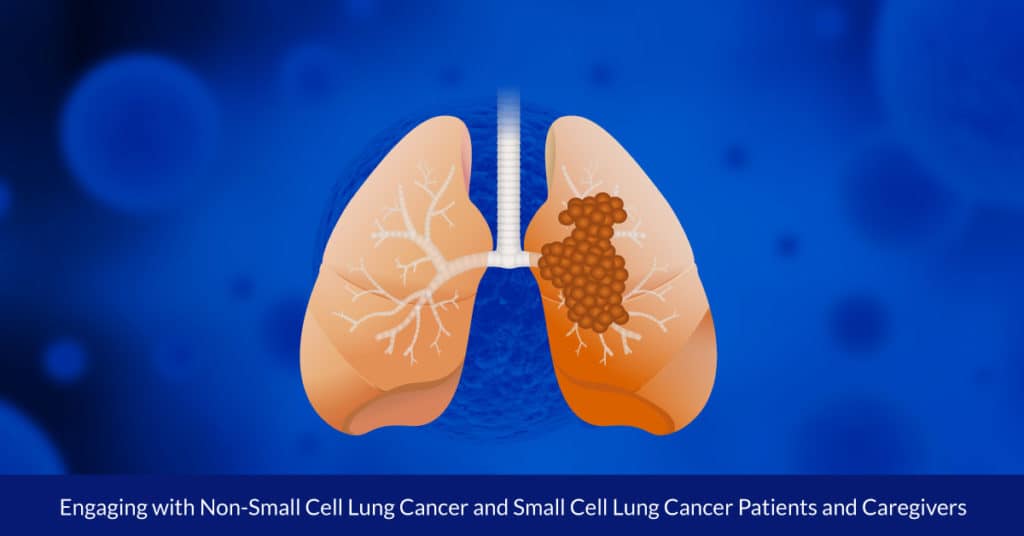
Engaging with Non-Small Cell Lung Cancer and Small Cell Lung Cancer Patients and Caregivers
By Kathleen Hoffman, PhD, MSPH
The word “Earth” doesn’t reflect the complexity and diversity of the planet. Similarly, the term “lung cancer” only identifies the location of the cancer. There are two general categories, non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC), differentiated by cell size, characteristics, treatments and prognosis. Genetic research continues to differentiate lung cancers at a molecular level, revealing subtypes within those categories, creating opportunities for increasingly targeted therapies. For example, since eight driver mutations have been identified, indicated treatments are available for 33 percent of lung cancers.1
With these advances, biomarker testing is now the standard of care for many cancers. For those with any of the eight driver mutations, targeted therapies improve outcomes when compared with chemotherapy and immunotherapy. However, according to two recent studies, biomarker testing for non-small cell adenocarcinoma, which includes NSCLC, is underutilized by oncologists and used differently by race among those who did receive it.1,2
The studies were presented at the 2021 ASCO (American Society for Clinical Oncology) annual meeting. The first surveyed 1,000 oncologists spread throughout the United States, and found that “…less than 50% of patients were tested for five major biomarkers (ALK, BRAF, EGFR, PD-L1, and ROS-1),” despite the importance of biomarker testing. While 90% of the 3,474 patients had been tested for one biomarker, only 46% had received all five biomarker tests.2,3
The second study of 14,768 patients’ data found that while about 70% of both white and black patients treated for NSCLC between 2017 and 2020 received at least one single molecular test or comprehensive genomic analysis, only 39% of black patients received next generation sequencing (NGS), compared with 50% for white patients. The implications are that advanced testing is underutilized for everyone with NSCLC, and used even less for African Americans.4
I’m 12-year lung cancer survivor. I’ve done pretty well over the years but am now experiencing my fourth recurrence. I’ve had NSCLC with the KRAS mutation for most of my journey but my cancer has now mutated from KRAS to ERBB2 (Her 2/NEU)… Does anyone have this mutation and if so, what was your treatment?
With less than 200,000 cases diagnosed in the United States per year, small cell lung cancer (SCLC) is considered rare. SCLC accounts for only 15% of lung cancers, spreads more quickly than NSCLC, and has a 5-year survival rate of less than 7%. Unlike NSCLC, SCLC originate in neuroendocrine cells in the lungs. While NSCLC studies identified subsets and biomarkers that support targeted treatment, SCLC remained elusive, leaving it to be treated as a homogeneous disease for over 40 years. Immunotherapy created some — but hardly enough — improvement.5,6,7,8
Now, breakthroughs in research are identifying subtypes of SCLC, which is the first step toward providing individualized treatment. Researchers discovered that four subtypes could be identified by their differing use of transcription factors and immune pathway activation. With this information, therapeutic vulnerabilities of each individual subset can be found. For example, one subgroup called “inflamed SCLC” features a higher level of immune checkpoints, indicating that this kind could be vulnerable to immunotherapies. 9
The search for answers and support are common among members. One Inspire member described his/her mother’s treatment for SCLC:
They started her on chemo (treatments) and immunotherapy (treatment) [date] which she will be getting every 3 weeks. This is the “standard of care” but wondering if there are more options out there or clinical trials or a specific hospital/cancer treatment center that people recommend?
An NSCLC survivor asked:
I’ve been wondering if it would be beneficial to have my tumor tested for biomarkers after I’ve already been through surgery and adjunctive chemotherapy? I was adenocarcinoma, stage 2A now and have been urged by some stage 1 folks to have the testing done, but I’m not sure what their reasoning is. Is it so that if the cancer comes back the test will already have been done? But what if it is a different type?
The Inspire audience interested in lung cancer is estimated to be over 181,000 people. The audience size specifically for NSCLC is estimated at 143,000+ who are responsible for the 931,000 posts on this topic. The audience size for SCLC reflects the rarity of the disease, 22,000 people with 18,000 posts. Both are a rich source of data about the expectations and concerns of patients and caregivers.
Inspire offers a trusted community to patients and caregivers. Our goal with this blog, this website and our content is to provide the life science industry access to the true, authentic patient voice. In so doing, we support faithful operationalization of patient-centricity. Take a look at our case studies, eBooks and news outlet coverage.
References:
1 https://corp.inspire.com/resource/analysis-online-patient-discussions-inform-biomarker-lung-cancer-content/
2Goodman, A. “More Widespread Biomarker Testing for NSCLC in Oncology Practices and More Testing in Black Patients: An Urgent Priority.” The ASCO Post. June 8, 2021
3Robert, N.J. et al. “Biomarker tissue journey among patients (pts) with untreated metastatic non-small cell lung cancer (mNSCLC) in the U.S. Oncology Network community practices.” ASCO Annual Meeting. Abstract 9004. Presented June 4, 2021.
4 Bruno DS et al. “Racial disparities in biomarker testing and clinical trial enrollment in non-small cell lung cancer.” 2021 ASCO Annual Meeting. Abstract 9005. Presented June 4, 2021.
5 Basumallik N et al. “Small Cell Lung Cancer.” StatPearls. July 17, 2020.
6 Ciubka, B. “Small Cell Lung Cancer vs. Non-small Cell Lung Cancer: What’s the Difference?” NFCR blog post. November 4, 2020.
7Zhang B et al. “New Therapies and Biomarkers: Are We Ready for Personalized Treatment in Small Cell Lung Cancer?” American Society of Clinical Oncology Educational Book 41 (May 13, 2021) DOI: 10.1200/EDBK_320673 .
8 Ness E. “No Small Challenge: Emerging Therapies in Small Cell Lung Cancer.” CURE® Lung Cancer 2021 Special Issue, April 21, 2021
9Gay C et al. “Patterns of transcription factor programs and immune pathway activation define four major subtypes of SCLC with distinct therapeutic vulnerabilities.” Cancer Cell. Volume 39, Issue 3. March 8, 2021.