[vc_row][vc_column][mpc_textblock content_width=”100″ font_preset=”preset_0″ margin_divider=”true” margin_css=”margin-top:20px;margin-bottom:20px;”]Suffering Through the Opioid Crisis: The Language of Chronic Pain
[/mpc_textblock][vc_row_inner][vc_column_inner][mpc_image image=”11778″ image_size=”large” force_fullwidth=”true” image_opacity=”100″ image_inner_border_gap=”0″ effect=”none” image_hover_opacity=”100″][/vc_column_inner][/vc_row_inner][mpc_textblock content_width=”100″ font_preset=”preset_2″ margin_divider=”true” margin_css=”margin-top:20px;margin-bottom:20px;”] By Claire Harter, MA
Market researchers in the pharmaceutical industry need to know their audience – their unmet needs, language, and experiences. Recent research in chronic pain at Inspire reveals the lexicon of chronic pain patients and their experiences with treatment.
Pain Management History
Documented widespread under-treatment of pain was a major medical health problem prior to the year 2000. The World Health Organization’s Cancer Pain Monograph detailed poor pain management of cancer and post-operative patients in 1986. Multiple publications throughout the 1990s on inadequate assessment and under-treatment of cancer-related and chronic pain heightened awareness of the problem. In 2001, the US Congress declared 2001 to 2010 the “Decade of Pain Control and Research.”2
Concern arose in 2015 when the life expectancy in the US declined from 78.8 years in 2014 to 78.7 years while the life expectancy of other industrialized countries life expectancy increased. In 2016 and 17, life expectancy in the US declined again to 78.5. Government researchers determined the cause: opioids. The CDC submitted guidelines for opioid use in 2016.3
Unfortunately, for those living with chronic pain, these guidelines may have done more harm than good. In a 2019 New England Journal of Medicine commentary, the CDC stated,
“…some policies and practices purportedly derived from the guideline have in fact been inconsistent with, and often go beyond, its recommendations. A consensus panel has highlighted these inconsistencies,5 which include inflexible application of recommended dosage and duration thresholds and policies that encourage hard limits and abrupt tapering of drug dosages, resulting in sudden opioid discontinuation or dismissal of patients from a physician’s practice. The panel also noted the potential for misapplication of the recommendations to populations outside the scope of the guideline. Such misapplication has been reported for patients with pain associated with cancer,5 surgical procedures,5 or acute sickle cell crises. There have also been reports of misapplication of the guideline’s dosage thresholds to opioid agonists for treatment of opioid use disorder. Such actions are likely to result in harm to patients.”4
How have the changes in pain management over the last twenty years impacted chronic pain patients?
Inspire’s Work with FDA
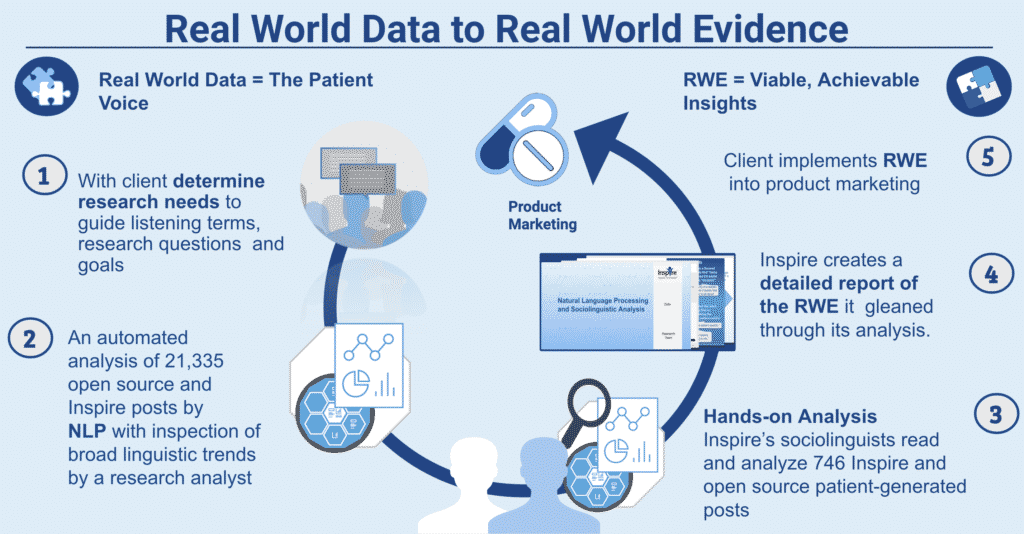
In 2019, Inspire obtained a grant from FDA to conduct Natural Language Processing (NLP) and hands-on sociolinguistic analysis of two years of online Inspire and open source public posts discussing chronic pain. The goal? To learn the impact of chronic pain and the “opioid crisis” on patients suffering from chronic pain.
The results of this research reveal how patients converse about chronic pain and pain relief treatments online. For example, one patient member wrote,
“… still, the pain worsens. Like a swarm of bees, stinging so intense it is hard to imagine.” – Inspire, Patient, CRPS”
The complete report to FDA describes, through an exploration of the patient journey, the top challenges, successes, and perceptions of these patients.
An initial “chronic pain” search yielded 4 million posts. Narrowing to an analysis-ready data-pull of over 21,000 posts, Inspire’s analysts provided structured RWE, based on the unstructured Real World Data, classifying the data into four distinct themes:
1) Disease perceptions and pain points: Focused especially around quality of life and descriptions of pain.
2) Treatment perceptions and unmet need: Focused on opioids, narcotics (41.3% of treatment mention) medical devices (22%) and alternative treatments (36.2%, divided into alternative activities, such as yoga, and alternative items, such as supplements).
3) Patient resources and information sharing: Discusses the chronic pain patients need to know what is causing their condition. Sometimes these patients feel the need to advocate for themselves with their healthcare providers and look to each other for information. Chronic pain patients also share news around the opioid epidemic such as press releases and petitions supporting chronic pain patients’ rights.
4) Chronic pain in the public eye: Covers the discrimination chronic pain patients feel, not just from their condition but also ageism, racism and gender discrimination. Chronic pain patients prefer the word “dependence” rather than “addiction.” Most of their social media posts avoided or overlooked indications of addiction in other’s postings. Chronic pain patients share information about active legislation and about contacting local members of congress to change the situation.5
Today, we share our first case study discussing the real language of pain: How chronic pain patients communicate about it.
[/mpc_textblock][/vc_column][/vc_row][vc_row css=”.vc_custom_1483606399832{padding-top: 20px !important;padding-bottom: 20px !important;}”][vc_column][vc_row_inner][vc_column_inner width=”1/2″][mpc_textblock content_width=”100″ font_preset=”preset_2″ margin_divider=”true” margin_css=”margin-top:20px;margin-bottom:20px;”]Download this case study, “Linguistic Analysis and Audience Insights: How Chronic Pain Patients Communicate About Pain”
[/mpc_textblock][mpc_button preset=”preset_1″ block=”true” url=”url:https%3A%2F%2Fcorp.inspire.com%2Fresource%2Fchronic-pain-audience-insights|title:Linguistic%20Analysis%20and%20Audience%20Insights%20||” font_preset=”preset_1″ font_color=”#ffffff” font_transform=”none” font_align=”center” title=”Download this case study” icon=”fa fa-angle-right” icon_color=”#ffffff” icon_size=”14″ icon_effect=”stay-left” icon_gap=”20″ background_color=”#084a8e” border_css=”border-radius:2px;” padding_divider=”true” padding_css=”padding-top:10px;padding-right:20px;padding-bottom:10px;padding-left:20px;” margin_divider=”true” margin_css=”margin-top:30px;” hover_font_color=”#ffffff” hover_icon_color=”#ffffff” hover_background_color=”#116eba”][/vc_column_inner][vc_column_inner width=”1/2″][mpc_image image=”11775″ image_link=”url:https%3A%2F%2Fcorp.inspire.com%2Fresource%2Fchronic-pain-audience-insights|title:Linguistic%20Analysis%20and%20Audience%20Insights%3A%20How%20Chronic%20Pain%20Patients%20Communicate%20About%20Pain||” image_size=”large” image_opacity=”100″ image_inner_border_gap=”0″ effect=”none” image_hover_opacity=”100″][/vc_column_inner][/vc_row_inner][flipbook-shelf ids=”humanizing_the_brand_experience, insights_from_engaged_patients, expert_by_experience_2016, expert_by_experience_2015, expert_by_experience_2014, case_studies_using_multimodal_research, case_study_prostate_cancer_consumer_support_group_survey, case_study_sleep_disorders_private_research_community”][mpc_callout layout=”style_8″ title_font_preset=”preset_5″ content_width=”100″ content_font_preset=”preset_2″ icon_disable=”true” background_color=”#e8e8e8″ border_css=”border-width:5px;border-color:#d3d3d3;border-style:solid;” padding_css=”padding:15px;” mpc_button__preset=”preset_1″ mpc_button__block=”true” mpc_button__url=”url:%2Fresources|||” mpc_button__font_preset=”preset_1″ mpc_button__font_color=”#ffffff” mpc_button__font_transform=”none” mpc_button__font_align=”center” mpc_button__title=”Learn More” mpc_button__icon=”fa fa-angle-right” mpc_button__icon_color=”#ffffff” mpc_button__icon_size=”14″ mpc_button__icon_effect=”stay-left” mpc_button__icon_gap=”20″ mpc_button__background_color=”#47aff3″ mpc_button__border_css=”border-radius:2px;” mpc_button__padding_divider=”true” mpc_button__padding_css=”padding-top:10px;padding-right:20px;padding-bottom:10px;padding-left:20px;” mpc_button__margin_divider=”true” mpc_button__margin_css=”margin-top:10px;” mpc_button__hover_font_color=”#ffffff” mpc_button__hover_icon_color=”#ffffff” mpc_button__hover_background_color=”#116eba”]Inspire offers a trusted community to patients and caregivers. Our goal with this blog, this website and our content is to provide the life science industry access to the true, authentic patient voice. In so doing, we support faithful operationalization of patient-centricity. Take a look at our case studies, eBooks and news outlet coverage.[/mpc_callout][/vc_column][/vc_row][vc_row][vc_column][mpc_textblock content_width=”100″]References
1U.S. Department of Health and Human Services (2019, May). Pain Management Best Practices Inter-Agency Task Force
Report: Updates, Gaps, Inconsistencies, and Recommendations. Retrieved from U. S. Department of Health and Human
Services website: https://www.hhs.gov/ash/advisory-committees/pain/reports/index.html
2http://www.npcnow.org/system/files/research/download/Improving-the-Quality-of-Pain-Management-Through-Measurement-and-Action.pdf
3DeWeerdt, S. (2019, September) Tracing the US opioid crisis to its roots
Understanding how the opioid epidemic arose in the United States could help to predict how it might spread to other countries.Nature. 573:S10-S12. doi: 10.1038/d41586-019-02686-2
4 Dowell, D. Haegerich, T. Chou, R. (2019). No Shortcuts to Safer Opioid Prescribing, N Engl J Med. 380:2285-2287. DOI: 10.1056/NEJMp1904190
5Inspire Report to FDA: Social Listening for Patient Perspectives on Chronic Pain: Updated Final Analysis Report
January 27, 2020
[/mpc_textblock][/vc_column][/vc_row]