Video Vignettes: Through Their Own Eyes: Thyroid Cancer
Inspire asked its members if they would share their stories by video in a project called Through Their Own Eyes. Many did, and we have shared a number of these videos.(See links below)*
Today, we share a video by a member of the ThyCa: Thyroid Cancer Survivors Association Thyroid Cancer Connect Support Community on Inspire who, together with other members, wrote a book, After the Diagnosis: Medullary Thyroid Cancer.
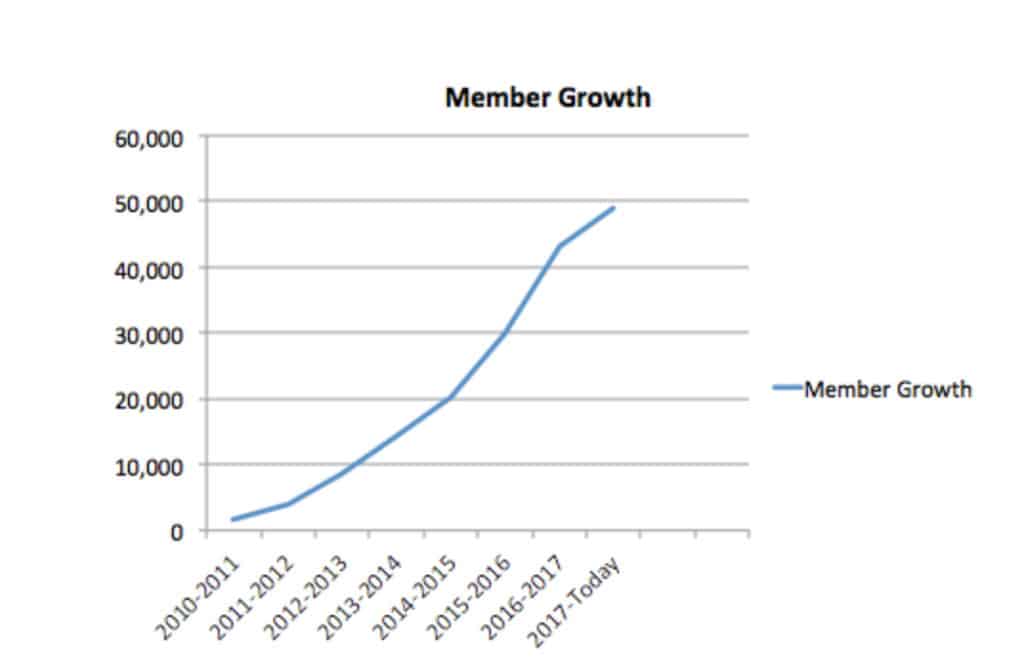
Thyroid cancer is a rare cancer. The American Cancer Society estimates in 2018 there will be about 54,000 new cases of thyroid cancer and around 2,000 deaths from thyroid cancer in the US. 1 Inspire’s thyroid cancer support community has, to date, over 49,000 members.
Types of Thyroid Cancer
Differentiated thyroid cancers – papillary, follicular and Hurthle (or oxyphil) cell cancer – make up the majority (90%) of thyroid cancers. These are cancers of the follicular cells, the producers of thyroid hormone. On average, differentiated thyroid cancers grow more slowly and are found at earlier stages.
Undifferentiated follicular cells typify anaplastic thyroid cancer (ATC), a very rare and aggressive form of the disease. Only around 600 people in the US are diagnosed with ATC each year. Although the cause is not known, some believe that existing follicular or papillary cancer will morph into this aggressive form. Patients with ATC have normal thyroid hormone numbers making ATC hard to detect early. It progresses quickly and is often metastatic when it is found.
Parafollicular cells (also called C cells), the cells of the thyroid responsible for producing calcitonin, a calcium-regulator hormone, constitute Medullary thyroid cancer (MTC). Around 3 to 5 percent of thyroid cancers are of this type. MTCs are either familial, sporadic, meaning there is no known reason for the cancer occurring or part of a complex disorder called Multiple endocrine neoplasia (MEN I or MEN II). Mutations on the RET gene on chromosome 10 cause both the familial form and the MEN I and MEN II forms.
Surgery is the first line of treatment for all thyroid cancers. Radioactive iodine, a treatment options available to people with ATC and differentiated thyroid cancers, is not an option for people with medullary thyroid cancer because the cells involved do not utilize iodine.2,3
ThyCa: Thyroid Cancer Survivors’ Association Thyroid Cancer Connect Support Community on Inspire
The Thyroid Cancer Connect Support Community on Inspire started in November, 2010. In its first year, the community grew to over 1,500 members and as of November 2017, it had over 43,000 members.
Inspire’s partner, ThyCa: Thyroid Cancer Survivors’ Association, actively shares updates with community members. There have been over 377,000 posts in the community since its inception. Members communicate valuable information, including practical ideas on what to do after surgery.
“If you have to swallow, sneeze, cough – tilt your chin down, as it will lessen the strain from the discomfort after the surgery.”
The Good Cancer?
Some patients with thyroid cancer hear from physicians, nurses and the general public, that thyroid cancer is “the best cancer to get.” This sentiment offends some.
“I heard the ‘it is the best cancer to get if you got cancer,’ line as well. I also used the line to reassure my family and friends it was no big deal. I even had myself convinced it was no big deal. I know now that is not true. I tried really hard not to think about the fact I had cancer, because it was the good one. But since my surgery two years ago, my life has been a roller coaster ride….Now when I hear someone say ‘oh the good one to have’ I have to stop myself from slapping them in the face.”
“I share your frustration. I know the doctor and people keep saying it’s the “good” cancer but I still feel like crap.”
“We are not alone in this sort of victimization by minimization! Other people are told their cancers are “good cancers” or not cancer at all. The people who tell us all this…do not realize they have damaged their credibility with their patients. A little empathy would work wonders.”
The “good cancer” sentiment confuses others. Having heard the “good cancer” statement often, one member, began to wonder if they needed to go through treatment.
“We hear often that thyroid cancer is a good cancer and it does not kill. Any proof or statistics showing that this cancer does not kill? If it does not, why do we go through all sorts of treatments to get rid of it ?”
Another member clarified the true nature of thyroid cancer.
“Unfortunately, while there is a current uptick in documented thyroid cancer cases around the country, there is still a public (& sometimes medical) perception that our type of cancer is not potent or bad or deadly. In general, I think it is…a result of less publicity. However, physicians in our area of study should be very aware & should never minimize the plight of treating thyroid cancer… if they are worth a darn.
Based on __#___ major surgeries, ____#___ mc RAI, and a truckload of labwork/drs appts/scans, I can confidently say thyroid cancer is no easy or good cancer. I would describe it as a cancer demanding great perseverance & patience… not just because of potential surgeries & other treatments, but also because of the “juggling” to get the right dosage of hormone replacement medication. Also, I know, as many on this board do, thyroid cancer has every potential of being deadly like all other malignant cancers. Metastasis from the thyroid to nearby organs or bodily-transport systems is a very real possibility. Even when successfully treated, this cancer can reoccur years down the road. And general oncology tells us if thyroid cancer is left untreated or is unsuccessfully treated, metastasis to bone or lung can occur in the worst of cases… and then it gets really challenging. Thyca deserves great respect & serious consideration as any other cancer.
So, yes, I would say it is very, very important to go through the hurdles to properly treat your thyca in hopes of getting rid of it. I encourage you to do so with a vengeance and with a medical care team who is skilled, experienced, empathetic, and available. A solid thyca physician not only focuses on the positive but also acknowledges the potential threat thyroid cancer poses if not treated appropriately. I hope you do what you need to do to pursue it, hunt it down, & stomp it in the ground.”
Members with rarer thyroid cancers are also there for each other:
“Ask me anything. Us (We) meddies [patients with Medullary Thyroid Cancer] are family!”
When a member asked others, “What have I done to deserve this?” the reply from one member was,
“I would not blame yourself, you never did anything….There likely are many causes of thyroid cancer…but likely we may never know which ones caused it. It is possible we were exposed to radon gas, or our vitamin D remained low making a tough time for the thyroid perhaps, or many other possibilities none of which you did or deserved.”
Upon getting a diagnosis of anaplastic thyroid cancer, a new member asked,
“Can anyone expect to live longer than a year after diagnosis?”
They received informed advice:
“Never give up hope! It’s really, really a tough go and hard not to be down, but remember there are always exceptions to everything. I…have heard of people living with ATC for several years. I was diagnosed about 2 years ago. Be your own advocate and get involved as much as you can. You mention options you don’t have, but have they talked to you about anything that can happen for you? Are you seeing an expert in ATC? I cannot stress the importance of finding someone who KNOWS this cancer and has a good, proven track record. And – someone you trust and respect. Have you thought about getting your tumor typed for mutations? This might help with some treatments targeted for you.”
Patients with rare cancers are often difficult to find. Inspire has robust communities of patients with rare cancer with extensive user generated content. Read about another rare cancer community that has engaged in research to accelerate medical progress by downloading the case study. Contact us to learn how to connect with Inspire members affected by rare cancers.
Inspire offers a trusted community to patients and caregivers. Our goal with this blog, this website and our content is to provide the life science industry access to the true, authentic patient voice. In so doing, we support faithful operationalization of patient-centricity. Take a look at our case studies, eBooks and news outlet coverage.
References:
1https://www.cancer.org/cancer/thyroid-cancer/about/key-statistics.html
3https://rarediseases.org/rare-diseases/thyroid-cancer/
*Other Video Vignettes:
Video Vignettes: Through Their Own Eyes: Living with Ostomy
Video Vignettes: Through Their Own Eyes: Idiopathic Pulmonary Fibrosis